I saw my rheumatologist for a three month follow-up recently. Incidentally, the day before my 40th birthday. Do I know how to get a party started or what? While I was sitting in the waiting room, two well dressed ladies came in and asked the receptionist if it would be possible to see my doctor. They were clearly drug representatives packing freebies. I had already been waiting forty-five minutes at this point, as had the gentleman a few seats away from me. I could not help but hope the drug reps were seeing the doctor after me.
Within five minutes, they were called to come back. I said to the gentleman near me, “I wish we were called that quickly.” He agreed and we began to talk. It was nice to swap personal health facts and experiences with someone that has dealt with wacky pain and inflammation. It was nice because he gets it and because we both had compassion for what the other has endured. He was not much older than me, drives a truck for Walmart, had a knee require surgery, soon after bodily joint pain and stiffness entered the scene and for the past few years he has been on methotrexate and a biologic that he self injects, and had a second knee surgery. The drugs are not getting the job done and he lives in pain.
I told him my body really let go after my fourth c-section and because I was nursing a baby, I researched alternative approaches. I shared with him the importance of looking at what you eat. He was surprised to hear that eliminating certain foods or chemicals can help take a load off your system. He had never heard that sugar was inflammatory. (Not only that–it’s like crack, people! Try to give it up for a month and tell me how you do. 🙂 ) I told him that I have done two different approaches with antibiotics. The first was nine months long, tough at the outset, progress was very gradual but awesome, and following it, I was drug-free and functioned quite well for a year and a half. Praise God. Now I have begun a second protocol and have been at it for a year, things are much better now than a year ago. He had never heard of the approach. I told him to check out the Road Back website. He was very interested and hopefully encouraged by the fact that I had experienced positive results. He was there to see my doctor after me. When I saw my doctor, I let him know his next patient might have questions. 🙂
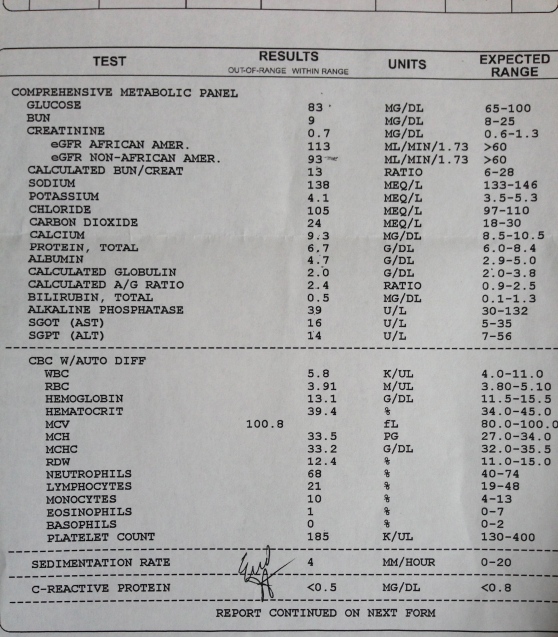
Here are my current lab results from 10/2013:
Not bad, eh? Except for that MCV number. My doctor said that meant enlarged red blood cells. “Which could mean what?” I asked. He said, “Could be thyroid, but we’ve checked that and you’re fine, alcohol is not a problem for you, labs show liver and kidney look good, could be your B12 or folate levels…let’s get that checked today and I will have the nurse call you with the results.”
Here’s a tip for anyone coming up on a birthday and a note to self. Do not consult with Dr. Google regarding anything about your health until waaaayyyy after your birthday! I couldn’t help myself and looked for information about enlarged red blood cells. I’m not going to even write about some of the things I read about.
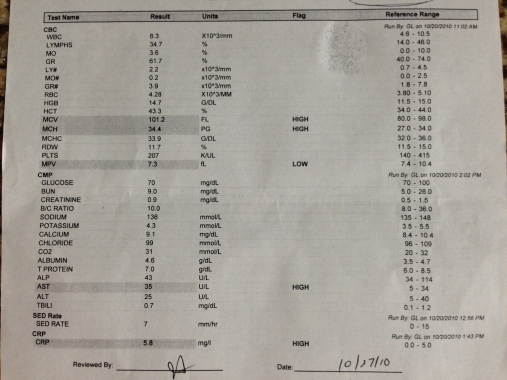
I remember seeing the MCV number high a long time ago on my lab results, in addition to MCH, but I recall my doctor not seeming concerned. I dug through my copies of blood work going back three years. The number has been up there for the past three years for both MCV and MCH. Interesting to me that it has my doctors attention now.
Lab results from three years ago (10/2010):
In looking at my lab results from my primary care doctor, I discovered that my B12 and folate levels looked good two years ago when they were checked and I have supplemented with a multi-vitamin daily since then and have maintained a healthy, whole-foods diet. I am guessing my levels will still be fine.
My doctor originally told me that he would keep me on minocycline for up to a year. I’ve passed the one year anniversary and was pleased that he didn’t mention taking me off and told me to schedule a follow-up three months from now. I am going to continue the minocycline indefinitely for now, as well as the sulfasalazine. I realized I would not see my doctor until the new year (hopefully won’t have to before) and wished him a Happy Thanksgiving, Merry Christmas and Happy New Year before going next door for more blood work.
Just for kicks, I did an online search today for information about long-term antibiotic therapy and this came up on page one of my search hits from Doctor Oz:
http://www.doctoroz.com/blog/jacob-teitelbaum-md/antibiotics-helpful-rheumatoid-arthritis
Thank you, Doctor Oz, for spreading the word!
And this:
http://recoveringarthritics.blogspot.com/2009/11/three-recovering-arthritics.html
She might as well be me talking!
I also searched the list of abstracts presented recently at the American College of Rheumatology Annual Meeting in San Diego in hopes that this treatment is being investigated further. Unfortunately, not really. To me, it is heart breaking. I found numerous studies involving biologic drugs, however.
I found the following chart in one of the abstracts. The chart displays the average co-pay for drugs used for RA under Medicare–$250-$650 for a biologic. Plain crazy. I scrolled down and found minocycline–$7.
So, what are the chances of pharmaceutical companies funding research studying long-term antibiotic protocols and their role in killing what can trigger certain autoimmune diseases? I’m thinking next to none because they stand nothing to gain! Sad beyond measure.
Antibiotics as a treatment option are not being offered as readily as biologics, if even at all. Take the patient I spoke with in the waiting room for example. We have the same rheumatologist and he had never heard of antibiotics as a possibility. And he has been dealing with wonky joint pain and inflammation for a few years now. Antibiotics have certainly not been the end all be all for me. And they come with their own scary list of side effects. But my journey with them has changed my life for the better and it is important to me to share that in the hopes it could help someone else.
Unfortunately, there is a great deal of information out there that our doctors are not telling us about. I have never had a medical doctor talk to me about what I eat and its role in disease, or the importance of managing stress and its impact on my body.
| Table. Coverage for Rheumatoid Arthritis Drugs in U.S. Medicare Part D Plans. | |||||
|
Drug |
Plans covering drug (%) |
Plans covering drug without prior authorization (%) |
Plans Charging Percent Co-insurance (%) |
Mean Co-insurance (%) |
Average Copay Mean (SD) ($) |
| Biologic | |||||
| Abatacept |
54 |
4 |
100 |
30.1 |
601 (22) |
| Adalimumab |
100 |
7 |
100 |
30.0 |
583 (12) |
| Anakinra |
40 |
4 |
100 |
29.9 |
517 (19) |
| Certolizumab |
59 |
1 |
100 |
29.6 |
650 (16) |
| Etanercept |
100 |
7 |
100 |
30.0 |
547 (11) |
| Golimumab |
42 |
1 |
100 |
29.6 |
580 (17) |
| Infliximab |
100 |
7 |
100 |
30.0 |
255 (5) |
| Rituximab |
100 |
8 |
87 |
29.5 |
611 (25) |
| Tocilizumab |
40 |
1 |
99 |
29.7 |
335 (14) |
| . | |||||
| At least 1 biologic DMARD |
100 |
9 |
87 |
30.3 |
275* |
| . | |||||
| Non-biologic | |||||
| Azathioprine |
100 |
34 |
10 |
18.1 |
7 (1) |
| Cuprimine |
60 |
60 |
59 |
30.6 |
83 (6) |
| Cyclophosphamide |
94 |
2 |
20 |
27.4 |
32 (3) |
| Cyclosporine |
100 |
12 |
22 |
25.1 |
34 (2) |
| Hydroxychloroquine |
100 |
100 |
10 |
18.1 |
5 (1) |
| Leflunomide |
100 |
100 |
13 |
19.3 |
11 (1) |
| Methotrexate |
100 |
85 |
13 |
19.8 |
5 (1) |
| Minocycline |
100 |
94 |
10 |
18.1 |
7 (1) |
| Sulfasalazine |
100 |
100 |
10 |
18.1 |
5 (1) |
| . | |||||
| At least 1 non-biologic DMARD |
100 |
100 |
11 |
18.2 |
4* |
| .*mean copay of least expensive drug covered | |||||
Here are studies discussing the use of minocycline for rheumatoid arthritis from pub med:
http://www.ncbi.nlm.nih.gov/pubmed/14528503
http://www.ncbi.nlm.nih.gov/pubmed/10047718
The following is taken from:
British Journal of Pharmacology © 2013 The British Pharmacological Society.
“Minocycline is a second-generation, semi-synthetic tetracycline that has been in therapeutic use for over 30 years because of its antibiotic properties against both gram-positive and gram-negative bacteria. It is mainly used in the treatment of acne vulgaris and some sexually transmitted diseases. Recently, it has been reported that tetracyclines can exert a variety of biological actions that are independent of their anti-microbial activity, including anti-inflammatory and anti-apoptotic activities, and inhibition of proteolysis, angiogenesis and tumour metastasis. These findings specifically concern to minocycline as it has recently been found to have multiple non-antibiotic biological effects that are beneficial in experimental models of various diseases with an inflammatory basis, including dermatitis, periodontitis, atherosclerosis and autoimmune disorders such as rheumatoid arthritis and inflammatory bowel disease. Of note, minocycline has also emerged as the most effective tetracycline derivative at providing neuroprotection. This effect has been confirmed in experimental models of ischaemia, traumatic brain injury and neuropathic pain, and of several neurodegenerative conditions including Parkinson’s disease, Huntington’s disease, amyotrophic lateral sclerosis, Alzheimer’s disease, multiple sclerosis and spinal cord injury. Moreover, other pre-clinical studies have shown its ability to inhibit malignant cell growth and activation and replication of human immunodeficiency virus, and to prevent bone resorption. Considering the above-mentioned findings, this review will cover the most important topics in the pharmacology of minocycline to date, supporting its evaluation as a new therapeutic approach for many of the diseases described herein.”
Found this on minocycline and ovarian cancer: