So sorry for dropping off the face of the earth after Christmas. I’ve continued to check on my fellow bloggers, however, and each of you are never far from my prayers.
It’s important to me to record what has been going on with my health before my memories fade. The past couple months have been a bit of a ride. The pain I’ve dealt with in my neck for some time now, escalated to a level I could barely tolerate one night. In trying to sort out what is going on in that area, I’ve had multiple visits to my rheumatologist, chiropractor and an acupuncturist. I’ve also had multiple visits with a neurosurgeon and two MRIs, with two more scheduled for July. One of which is for my lower back. Not crazy about the fact that my wellness team is growing. But I’m so thankful that I have a team of outstanding professionals aiding me in my battle for my health.
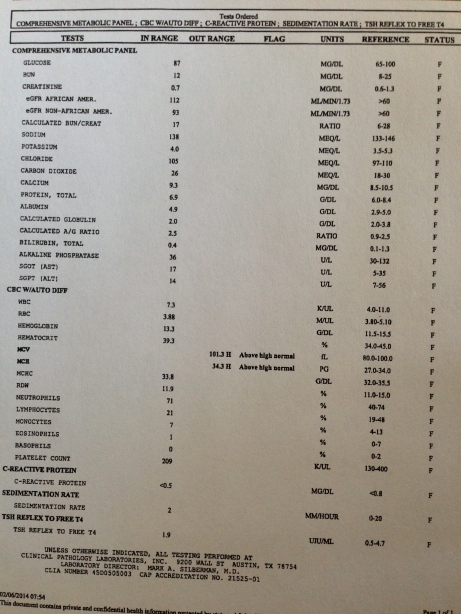
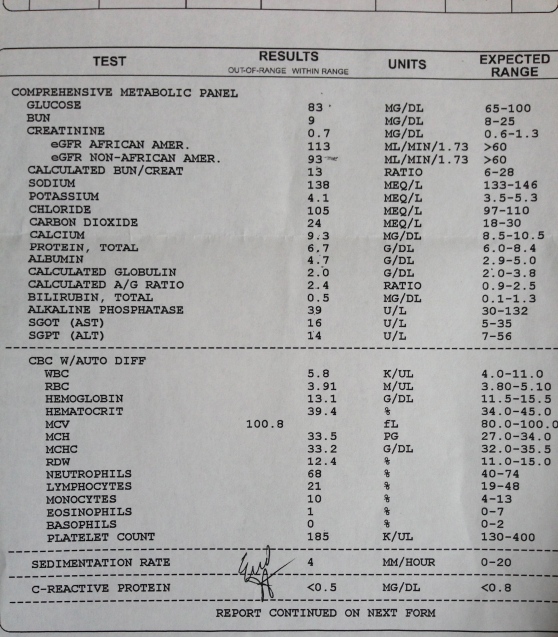
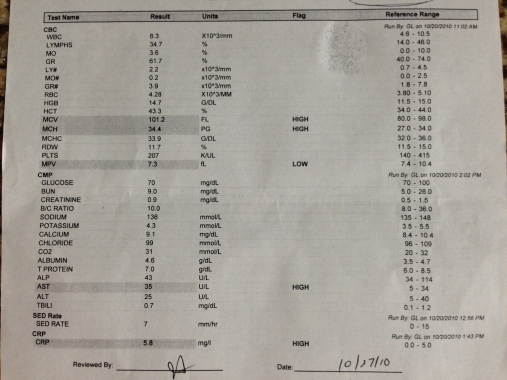
As far as my AP experience, I am pharmaceutical free as of last Friday. Feels strange and a little scary. It is still weird to wake up in the morning and not have to take an antibiotic. Weird and wonderful. I decided to continue past the six month mark with my antibiotic protocol and was just shy of completing nine months (I loosely had a year in mind). But recently, I began to think about quitting one of the antibiotics (azithromycin). From day one it caused me to experience increased pain levels the morning after I took it. I could basically count on hurting every Tuesday and Friday. Initially, I interpreted this as a good thing based on the fact that with AP it usually gets worse before things get better. But being almost nine months in and still experiencing increased pain got me wondering if it was such a good thing still. I also began noticing a bit of stomach distress after taking my azithromycin. And if that wasn’t enough, I saw my rheumatologist last week and saw my latest labs and they show my liver showing its first signs of distress. That’s enough to cause me to pull the plug.
I’m at peace with the decision and now I’m holding my breath to see how my body responds. In the meantime, I am trying to be very diligent about taking my numerous supplements and nourishing my body with good food since I notice a decline in how I feel when I slack off a bit. I am also making sure to do all I can to repopulate my gut with healthy bacteria.
I came up with a year of AP in my mind after extensive research. Even though my rheumatologist thought we should call it quits after six months, I felt strongly about pushing past six months. I felt like more work needed to be done in my body. Thankfully, he agreed to let me continue with careful monitoring every six weeks. He has really been a blessing. But I couldn’t shake the nagging feeling lately that it was time to drop one of the med.s. When I asked my doctor about this he said that I would need to quit the rifampin as well because on its own, one can develop antibiotic resistance. He also said that my body could be having a bad reaction to the azithromycin and that is why there is increased pain. So, just like that, I’m done with them both.
I asked him about trying antibiotics again in the future if my body starts to get out of control again. He said that is definitely a possibility and we would probably go the minocycline route.
At this moment, I am so glad I tried the AP route and would do it all over again. Something tells me I may have to. But hopefully, it won’t be for a long time, if ever. I am trying to stay focused and positive in my mind. I want my subconscious thoughts to be uplifting.
It helps to look back over my AP diary and my previous posts and remember how much pain I was in because it gives me a better perspective of the progress I’ve made. The pain I feel now in my joints feels like residual pain–tenderness left over from being attacked and inflamed. My feet still have tender spots, as does my right ankle. But I walk barefoot all over my house now and outside without any problem. Praise the Lord! Even if all of this is fleeting, it is fabulous right now.
It has also been several months now since a joint has swelled and I don’t wake up with morning stiffness (just achy joints). My progress has held steady in terms of my hands and feet, wrist and ankle. My neck and back are a different story. I wish I knew if they were separate issues or somehow related to my condition because they have both become worse and extremely painful at times.
As far as my pain in the neck–the night of January 30 almost sent me to the ER. I was struck with intense, mind numbing pain that evening in my neck and upper back. It was awful. I’ve never experienced anything like it and pray I never do again. I didn’t know what to do. It felt like lightening shooting down my spine. But the last place I wanted to end up was the ER in the middle of the night.
There was a lot of sobbing and cursing involved that evening. I tried to find relief first with an anti-inflammatory and a pain killer. But if offered no relief. In fact, it felt as if the pain level actually increased. I was afraid to move it hurt so much. I soon called the pharmacy to find out if I could take a third drug–a muscle relaxer. The pharmacist said they will sometimes do that in the ER and if my combo didn’t work–to go to the ER. It was hard to breath without lightening pain in my neck and upper back. I could not get in to any position that offered even a bit of relief.
It was only by the grace of God that I made it through the night. I was able to remain calm and tried to focus on my breathing and prayer, and at some point I actually fell asleep.
The following morning (and into the following week) every step or turn brought a strong shot of lightening pain. I could barely move without getting jolted. When I walked, I also heard an audible knocking sound coming from my neck. Completely creeped me out. The pain was different from anything I’ve ever experienced before. It felt electric and more intense than anything I’ve ever known.
I called my mom who lives roughly three hours away the next day for help. Praise God she has angel wings. She came and went multiple times over the coming weeks. I lost track of how many visits she made to help me care for my family. Her help, along with my sweet husband was priceless, because suddenly I couldn’t drive or do much of anything without the electric jolt zapping me.
The next call the following morning was to my rheumatologist to request an MRI. I’ve had x-rays taken of my neck recently and they showed nothing. It was time to get a closer look. When I saw my rheumatologist a couple weeks prior to the incident for a follow-up, I was in a great deal of pain in my neck area. He prescribed an anti-inflammatory, a muscle relaxer and a soft collar and said that the pain was probably not related to my disease.
After calling him to request the MRI, he asked to see me again first. Praise God, his office staff got me in the very next day. At this appointment he said that my pain might be related to my disease after all. He asked if I wanted a shot in the arm for pain and inflammation. Yes, please. I was given a shot of toradol which caused my arm to hurt like crazy all the way home, but worked like a miracle for 15 hours. He also offered me a prescription for a steroid dose pack (which I declined knowing that it would end up seriously ticking off my joints) and said he could give me a shot of Enbrel on the way out if I wanted. In retrospect, it is slightly alarming to me how trigger happy he was with a biologic. But it reminds me of how much pain I must have presented in. I know he was just trying to help in any way he could.
After leaving, I read his notes on the order for the MRI. They read–seronegative RA or possibly ankylosing spondylitis. He never made mention of the second disease to me during my appointment. I struggled with the possibility, but didn’t want to give in to the idea. Somehow it didn’t fit, yet somehow it easily could.
What is interesting to me is that I went to my PCP roughly three and a half years ago for crazy neck pain before ever seeing a rheumatologist for the first time. He referred me to physical therapy and said it was nothing to be concerned about. He never ordered x-rays or suggested anything else. When I saw the physical therapist, he said that based on the way I presented I should give up the kickboxing and running I was doing permanently. What?! I remember this news clearly because it broke my heart. I loved kickboxing. I didn’t understand. At the time I was healthy, active and fit. Why did I suddenly have to give up something I loved? He recommended PT a couple times a week for a couple months. I went diligently and found relief. But there was never any explanation for why my neck might be painful enough to send me to see a doctor. The only thing I could attribute it to was kickboxing.
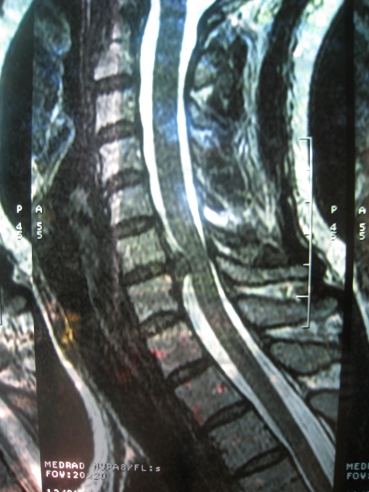
I had a follow up appointment with my rheumatologist to get my MRI results. He said there was a lot written for C5-C7, which is never good. My heart sank. But how bad could it be I thought? The radiologist’s report said there was a very large bulging disc pressing on my spinal cord and depressing the sac. My rheumatologist said that based on the report, it was very likely that I would need surgery and referred me to a neurosurgeon that he described as conservative. He said that out of the hundred or so patients he had sent his way, roughly ten had needed surgery.
I have to tell you that after years of being the girl that doesn’t show up on paper, I was relieved to finally show up on film–and in a big way. My doctor said he couldn’t believe I’d been living with this level of pain and offered me whatever I needed in terms of relief. I’ll never forget the way he looked at me after reading the radiologist’s report.

February 2, 2011
They got me in to see the neurosurgeon the very next day. When we got to the office, the waiting room was full–full of people that looked like they were hurting. I waited two and a half hours to see the doctor and I was the last patient to be seen.
The neurosurgeon finally came in, apologized for the delay and said he could help me. He said my situation was more extreme than most, but an open and shut case for him basically. He also said I was not in danger of paralysis in the meantime. All I needed to hear. Surgery was definitely the order of the day and he said he recommended that he perform it as soon as I would allow him to.
It was great to get a good look at my films for the first time. Anyone could see the disc bulging and pressing on the spinal cord. It was a crazy thing to see. He said there was some damage to the cord and asked if I was experiencing any numbness or tingling in my arms or legs. I told him that my hands had been falling asleep at night for quite some time. In fact, I mentioned this to my PCP when I saw him about my neck years ago and he said it was probably due to me having them in positions that caused this. Guess not.
The neurosurgeon said I would need an anterior cervical discectomy and fusion. Huh? The way I heard him explain this to me was, “Cut you open in the front above your collar bone, remove your entire disc, insert a disc composed of a dead person’s bones encased in an artificial plastic material, blah, blah, titanium plates and screws in your spine, blah, no neck movement for six weeks, no driving, lifting or bending for at least two, collar worn for six weeks.” Eek.
The neurosurgeon then led me down the hall to his nurses’s office and said if I chose, I could schedule the surgery with her. For some reason, my gut said to simply book it. For some reason, thoughts of a second opinion and further research weren’t a part of the equation. I just felt the need to move forward with the surgery so I could get on with healing.
In retrospect, I think there was a part of me that was thinking–there is actually something wrong with me that I am being told can be fixed. I’m so used to hearing–this is something you will have to deal with for the rest of your life. There is no cure and you will have to take drugs to attempt to manage it for the rest of your life as well. So, a prognosis for pain relief with surgery was in some strange and tiny way–a relief.
I can’t help but wonder if the problem with my neck is holding up greater progress with my hands and feet. It is certainly possible since the area of my spine affected is connected to my hands and feet. What if alleviating the problem with my neck takes a load off my hands and feet and I am able to cross a few more hurdles toward better health? A girl can dream, right?
I scheduled the surgery for their first opening and left with my head spinning, wondering how in the world my family would function with me out for two to six weeks. No neck movement for six weeks and zero activity for two? How was that going to be possible? I’ve never not done anything for two weeks. I felt overwhelmed.
I wrote what follows in February after I scheduled the surgery and stuck it in my drafts folder. (I have since cancelled the surgery.)
It’s very difficult to wrap my mind around what is to come. Unlike my last c-section (my 4th), which at times brought on fearful feelings before it occurred, I feel almost completely removed from what is about to happen. Just focused on getting through surgery, being the best patient I can be and moving on to recovery.
Does this mean that my neck issue is related to my disease or is it a separate issue? Neurosurgeon thinks they are separate issues, but my rheumatologist seems to be on the fence.
My oldest son brought home cards written by all of his classmates. Just seeing the stack of cards with my name on it made me cry. I realized in that moment how concerned my son was since he talked about it with his teacher and his class. I couldn’t even open the cards for a couple of days. I was too overwhelmed. But when I did, God’s power and love was unleashed through those kids.
There are a lot of people praying for me. When I stop to think about all of the people praying for me, I can’t help but cry. It just humbles you. I don’t always like asking for prayer. Maybe because it sometimes means there is a bit of a crisis going on. But I believe in the power of prayer with all my heart. And somehow, I have been able to get by this week without my mom being here. The pain is significantly less. That’s a praise report if you ask me and nothing short of a miracle considering how much pain I’ve experienced the past couple weeks.
(The following was written present day….)
Then I began to have second thoughts about the surgery. It led me to research it more extensively and seek a second neurosurgeon’s opinion (he looked at my MRI films and offered epidural pain relief, pain killers and said if that didn’t help that I should have an anterior cervical discectomy performed). I also made another appointment with the neurosurgeon scheduled to do my surgery. I had more questions now and more concerns.
At this point, I was managing to function at a decent level, but was not lifting my little guy or anything else heavy for that matter, and was taking it as easy as possible. I continued to get weekly adjustments (very gently) from my chiropractor and saw an acupuncturist. The pain was now more tolerable and my constantly interrupted sleep (due to pain) was something I accepted as par for the course.
My neurosurgeon was very understanding at the follow up appointment and said if I wanted to wait on surgery, that he wanted to have another MRI done in four to five weeks to make sure I wasn’t in any danger. I left feeling extremely grateful that I would get another look and thought–OK, time to work on healing. I wanted to see improvement in my follow up films. I remember praying a few days later, Lord, please allow me to see your work through my MRI films. I knew a lot of people were praying and I wanted to show them something awesome. I felt prepared for either situation though.
It makes me cry now thinking about my prayer because here is my second MRI. Huge improvement.

March 9, 2011
I have to show them side by side. Here is first one again. Ouch.

February 2, 2011
My neurosurgeon was amazed with my follow up MRI. He said he has never seen an improvement as major as mine happen so quickly. He was taking pictures of the first films I brought with me again with his phone to show his colleagues the improvement. Take all the pictures you want I thought. 🙂 He said that he had to eat his words in a sense because now my surgery was more optional than critical. But he still highly recommends that I have it done based on my age, condition, family demands, etc. He said that if I were his sister or his wife he would say, “Baby, you should really have this done.” He also said (without knowing anything about my faith) that when he goes before God, he would be at peace saying he had recommended I have this done. Heavy sigh….
When I think about the fact that my neck went crazy at the end of January and we are now into May, I am stunned. I know we all say time flies, but I feel as if time has warped. More so than ever it seems.
It is also very hard to believe that my oldest is completing his first year of middle school at a private school with a butt kicking curriculum in just a few weeks and two of my other boys will be through another whole school year. This has by far been the fastest a school year has ever flown by. Maybe because my husband took over driving my boys to school each morning a few months ago. Praise the Lord. I don’t know. But something has truly impacted my sense of time.
My youngest is also turning two this month. It seems like just yesterday that we had a big monkey birthday for him and a house full of children and adults. This year, I am planning on an intimate family gathering.
Since I have decided for now to not have surgery, I have to know what my limits are. When I start to feel less pain and have increased mobility in my neck and back, I push my limits (i.e. lifting, sweeping, bending, stooping) just a bit more to see what my new normal is and to attempt to determine if this is a doable normal for me. Doable in the sense that I can carry on, get things done and not limp along pathetically relying on others all the time. It has required getting used to a new level of pain, a new level of limitations. It’s amazing what we are capable of accepting as our new normal. And I have to accept it for simply what it is or I will turn into a resentful and unpleasant grump.
My other option is to give surgery a shot, to replace my God given disc with a mix of a dead person’s and an artificial material, a few long screws and a plate–which gives me the creeps. And quite honestly, I think that surgery is a crap shoot because it could bring relief, or it could even bring more pain if I don’t respond well to the procedure.
Of course, each time my neck and back flare up, I contemplate surgery because sometimes my new normal is pretty crummy. But thankfully, in the midst of this my energy level is good, my mind feels clear and my other joints feel the best they have felt in years.
Praying this finds you well. So many of you are on my heart and in my prayers.